Mothers around the world are dedicated to promoting the health and wellbeing of their children daily. Our partners change lives in their communities in sub-Saharan Africa every day, but one vital area of work that many people aren’t familiar with is the prevention of mother-to-child transmission of HIV, otherwise known as PMTCT.*
What is PMTCT?
A Miracle of Modern Medical Technology
Around the world, there were 1.3 million pregnant women with HIV in 2018, and all of them needed interventions for prevention of mother-to-child-transmission of HIV (PMTCT), according to the World Health Organization (WHO). Most young children who acquire HIV get it through their mothers – 86% of the 160,000 children in the WHO African region in 2018. In 2017, about half of the 180,000 children newly infected with HIV acquired it during breastfeeding, in some places more common than transmission through pregnancy (UNAIDS).
But thanks to the “miracle of modern medical technology,” mothers have the ability to effectively eliminate the risk of passing HIV to their unborn or newly born children! An HIV-positive mother can pass HIV on to her baby at any point during pregnancy, labor, or breastfeeding, so she needs HIV treatment for the health of her baby throughout this time. Without treatment, her likelihood of passing HIV to her child is about 15-45%, but with it, that risk can be below 5%. About 80% of all pregnant women who receive ART successfully prevent transmission of HIV to their children (WHO), a significant increase from 2010, when this was only 51% (UNAIDS)!
A Comprehensive Approach
The World Health Organization (WHO) recommends a comprehensive approach to PMTCT, well-supported by past research and practices in the field of HIV. There are three primary focuses for PMTCT programs that health organizations adopt due to the WHO’s guidelines:
1. Infant feeding for mothers living with HIV
Since some countries have other, perhaps more immediate, serious health risks for infants, many women are counseled to breastfeed their children even if HIV treatment is not available to them, although they should maintain ART treatment if possible. A large proportion of mothers gradually stop treatment after birth, which puts infants at risk of acquiring HIV during breastfeeding. Combining ART treatment with maternal and pediatric services can ease the burden on mothers to help them keep up their adherence to treatment.
2. Testing for HIV-exposed infants
If an HIV-exposed infant is given ART in its first twelve weeks of life, he is 75% less likely to die from an AIDS-related illness. Early infant diagnosis is essential to ensuring he does not acquire HIV, with testing between four to six weeks and again at eighteen months or when weaned off breastfeeding. Since this is such a critical time in a child’s development, the time it takes for these test results is another concern for PMTCT, and on-site testing has helped to overcome this difficulty. If infants quickly receive their results, they can begin their ART immediately when needed.
3. Immediate treatment for HIV-positive infants
HIV-positive infants and children who start treatment late are more likely to experience treatment failure, which is why it is so important to diagnose HIV as soon as possible. Among the 23 priority countries in 2016, four of them had treatment coverage of 60% or more. Tragically, about half of the infants with HIV who don’t receive treatment will die before their second birthday.
The Global AIDS Response
UNAIDS set proposed targets for the world’s response to HIV/AIDS by 2025, putting people at the center, especially those most at risk, such as young women, girls, and adolescents. However, the global response has been trending below the proposed targets since before the COVID-19 pandemic began.
UNAIDS also introduced Start Free Stay Free AIDS Free to inspire progress in HIV in 23 priority countries, including all of the countries in which our current partners operate: Ethiopia, Kenya, Malawi, and Uganda. In 2016, these countries were home to 87% of all children and adolescents with HIV globally, 87% of global new HIV infections among children, and 81% of new HIV infections globally in adolescent girls and young women (aged 10–24). That year, around 73% of the 740,000 women of reproductive age that became HIV-positive were in the priority countries, and primarily in sub-Saharan Africa, the region where 90% of all pregnant women with HIV live.
In 2017, just over half of the 1.8 million children living with HIV were receiving antiretroviral therapy (ART), which is life-saving and integral to keeping viral loads low and immune systems up; 110,000 children without access died due to AIDS-related illnesses the same year. As of mid-2019 almost every low- and middle-income country was fully implementing lifelong ART treatment, beginning immediately at diagnosis.
Barriers to PMTCT Support
lack of Understanding around the Virus
It is important for expectant mothers, especially in areas with a high prevalence of HIV, to understand what HIV is, and how to prevent it so they are more likely to get tested if they suspect they may be positive, and to access treatment if they are. Young girls and women (a high-risk group for acquiring HIV) are less likely to know their HIV status before giving birth to their child, a problem in itself because women diagnosed before pregnancy are much more likely to stick with their treatment.
Numbers from many African countries suggest women are three times more likely to acquire HIV during pregnancy and breastfeeding than women at different stages of life. While the reasoning for this statistic is not entirely clear, the realities of life for women in sub-Saharan Africa demonstrate that this is most likely due to lack of information about the virus, how it is transmitted, and how to utilize various methods of birth control even during pregnancy and breastfeeding to protect against exposure and infection. Though far too many women lack access to testing or reliable information, it is also common for women to purposely avoid it for fear of stigma and discrimination.
Stigma and Discrimination
Stigma and discrimination can be a serious deterrent to testing or receving treatment for HIV. Over 50% of mother-to-child transmissions can be attributed to the overall effect of stigma. Many women fear their families’ or partners’ reactions to learning their status and don’t seek the services they need to keep themselves and their babies healthy. This is a legitimate fear, when unfortunately there are women who are cast out of their homes or communities, abused, or experience another of the myriad of negative situations caused by stigma.
Even for women who do seek treatment, there are many healthcare providers that aren’t prepared to treat HIV-positive pregnant women, especially young women who may have more complicated circumstances like age of consent issues. Some women even experience maltreatment like denial of care and forced sterilization. Things like long wait times, lack of point-of-care testing, and separate mother and child facilities also make it a lot harder for women to realistically and reliably receive the care and support they need.
Gender Inequality
In many places, gender roles and local cultures influence women’s HIV care. In 2017, 29 countries required women to obtain consent of a spouse or partner, and where these services were available, they were mainly for married women. Since one of the most at-risk groups to HIV is girls and young women, this means that there is an even bigger gap in services for them, since they also have lower access to education, economic opportunity, and ability to negotiate rights with partners for example.
Many communities view pregnancy as a ‘woman’s affair’, however research suggests that male involvement in PMTCT is very beneficial to preventing new infant infections. Men who fear knowing their HIV status are less likely to be involved in PMTCT, and a 2018 study in Kibera, Kenya observed that male partners who took steps to be tested for HIV were more likely to let their partners participate in the program and supported adhering to it. So it is really important that men and fathers are taught the benefits of knowing their status and information about HIV.
The Good News
A number of countries have reached the elimination threshold for mother-to-child transmission of HIV, and since 2010, 1.4 million infections among children have been averted! There has been a 48% decline in new child infections among the 23 UNAIDS’ priority countries; at least nine of them reached or nearly reached the original target of 95% of pregnant women living with HIV on lifelong ART. These efforts have been particularly impressive in eastern and southern Africa where in 2017, an estimated 93% of these women were initiated or already on ART, and children acquiring HIV from their mother declined from 18% to 10% between 2010-2017.
Mentor mothers (mothers with HIV who mentor other HIV-positive mothers) play important roles in helping keep mothers in care and adhere to treatment, especially after they’ve given birth. In nine districts of eastern and central Uganda, facilities using the mentoring model had stronger retention in HIV care, a higher uptake of early infant diagnosis compared with other services, and a better psychosocial wellbeing of the mothers.
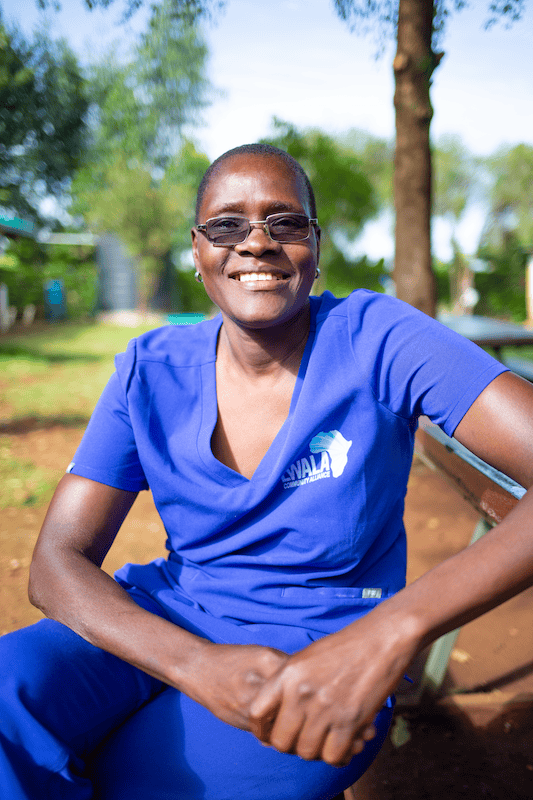
A Hero Without a Cape
Jane is a 52-year-old mother of five– three boys and two girls between the ages of 28 to 13, the fourth currently in college. She has been a mentor mother since 2013, and came to work with our partner Lwala Community Alliance in 2014. Since then she has mentored more than 300 HIV-positive women: “I talk to them one-on-one. I tell them my story, and some of them, most of them, can say, even today, even them, they can tell their stories because we talked and they realize that it’s just like a normal sickness. And they are okay with their statuses.”
Jane, like many women in her community, had a hard time in her journey discovering she was HIV-positive. She and her husband received their status in 2008 after he became sick and was tested for HIV at a nearby hospital in Nairobi. She chose to view their predicament positively after they were counseled together; she said she wouldn’t ask where the virus came from, but together they could pursue their new treatment. After taking their ARV medicine for two weeks, her husband refused his treatment and passed away.
For years Jane struggled to get by, moving back to her hometown in 2013 to live with her aunt, until 2014 when she interviewed and trained to become a mentor mother. With LWALA, she has helped hundreds of children graduate from their PMTCT program which is truly changing a generation in their area in Kenya. She explains,
“My purpose is to make sure that the mothers are receiving their treatment without missing, and their virals are suppressed for those who are breastfeeding and the pregnant mothers. Because for pregnant mothers, if they have a high viral load, sometimes they can feel sad they have given birth to a child who is HIV-positive. And those who are also breastfeeding, if their viral loads are not suppressed they can also infect the children…
I wanted to help these mothers, because all these days, back in the ‘90s, children were dying a lot because of this. Their mothers could go to the hospital to get tested. Even if they were tested, they couldn’t take the drugs. So I had to tell them the good thing about the mothers taking their drugs properly and for them… it is possible, they can deliver negative children. I had told them if they take their drugs properly, you cannot be sick, because you find that if you don’t take your drugs, if your immune system is low, you are vulnerable to get some diseases. So many diseases can put you down.”
PMTCT is especially important right now because COVID-19 severely interrupted HIV care and presented even more challenges to the international response to HIV/AIDS. We believe that everyone deserves access to health care and support, so we are thrilled to be a part of our partners’ empowerment of mothers and communities to provide their children the protection and care they need.
Today, you can help provide resources for moms in sub-Saharan Africa who are trying to build better lives for their children, and mothers like Jane trying to help as many women as they can. You can also help them keep their children healthy through basic life essentials like clean water, nutritious food, opportunities to improve their household income, medical treatment, and preventative care that will have immeasurable impacts on the wellbeing of entire families! Thank you so much for your support!
*Avert composed a wonderful report summarizing the global circumstances and response to PMTCT, in an in-depth and comprehensive way, which we used extensively here as a guide to distilling the complex, yet very exciting developments in the field.
More Stories:
Categories