People living with HIV continue to experience stigma around the world, and it remains an enormous problem in sub-Saharan Africa. Cultural beliefs and practices, along with limited access to information and education, combine to create an environment where stigma is one of the greatest barriers to accessing HIV treatment.
Many people refuse to be tested fearing that they will lose employment, family, friends, and more should they test positive. And even when they are brave enough to be tested, the necessity of remaining consistent with daily medications can be too much without a strong support system. These issues, along with legal barriers that can prevent them from accessing HIV services, increase their risk and create difficulties in accessing “effective, quality, and affordable HIV prevention, testing, and treatment services,” (WHO).
Programming must address stigma and discrimination in order to effectively solve the HIV/AIDS crisis in a community. So how do our African partners do this? Read on to find out.
STIGMA AND DISCRIMINATION
In order to explain how our partners address stigma and discrimination, we first must unpack those terms a bit.
Stigma
Stigma is a social process that occurs as a result of power relations in society. HIV/AIDS-related stigma can be described as a “process of marking or devaluing” people living with or associated with HIV/AIDS by one’s self, other individuals, groups, and institutions. It builds upon and reinforces existing prejudices and plays into and strengthens existing social inequalities – especially in reference to gender, sexuality, and race.
Types of HIV-Related Stigma:
-
Experienced: enacted through interpersonal acts of discrimination.
-
Perceived: perception of stigmatizing attitudes in the community or among healthcare providers.
-
Anticipated: fear of stigma, whether or not actually experienced.
-
Internalized: accepting experienced or perceived stigma as true and just.
-
Compound or layered: Intersecting stigmas faced by individuals who are part of multiple marginalized groups.
-
Secondary: stigma extended to family or other caregivers of stigmatized individuals.
These types of stigma can be caused by fear of infection, the financial impact of HIV being a lifelong health condition, poor productivity and longevity, and social norms around them, for example. And when people fear experiencing stigma or are experiencing it, that can lead to them avoiding HIV testing, life-saving care and treatment, and hinder them from spreading the word about the truth about HIV care to others around them who may be at risk.
DISCRIMINATION
Discrimination is the act of enforcing these differentials in power and control through things like stereotypes and prejudice. Caused by stigmatizing beliefs, discrimination is a range of practices, actions, and systems that cause some groups to be devalued and others to feel superior. Ultimately, stigma creates discriminatory practices which then reinforce stigma! Examples of things that might enable discrimination include: laws criminalizing HIV infection, unenforced protective laws for key populations, lack of access to personal protective equipment (PPE) in health facilities, and prevailing norms about populations most vulnerable to HIV infection.
>
“Ultimately, stigma creates discriminatory practices which then reinforce stigma”
For someone experiencing this discrimination, they may face things like social rejection, internalization of the stigma, secondary stigma for family and healthcare workers providing care to people living with HIV, failure to seek treatment and to use care, depression, lower levels of disclosure, lower quality of life, low self-esteem, lower treatment adherence, and isolation from others and community. All of these things can have serious negative repercussions in your life.
Stigma and discrimination doesn’t just stop at emotional and mental trauma. It can also cause people to remain in situations that put them at high risk of contracting HIV while avoiding HIV testing, engagement and retention in care, and initiation and adherence to medication. It can also be manifested through HIV-related laws and policies, workplace policies, and inadequate training for healthcare and other service providers. Together, these ultimately create higher rates of HIV infection, morbidity and mortality, social exclusion, and lower quality of life for huge numbers of people affected.
OUR APPROACH
At Blood:Water, we believe that people deserve a good quality of life regardless of their HIV status, and that everyone holds an equal right to life. Part of our criteria for selecting our local African partners is that they also operate under this belief and are working to make that a reality in their communities. Our partners have made some truly astounding strides in these areas over the years, and you can see some of the ways they did so last year in our 2020 Annual Report.
>
“To solve the crisis, we need to support people living with HIV”
The biggest way in which our partners work to address stigma and discrimination is through support groups, schools, and community institutions built around addressing them. Our focus in HIV revolves around communities, because to solve the crisis, we need to support people living with HIV, prevent further transmission, and build health systems that better address community needs. Because our partners are the experts on their communities, we make sure that they have the flexibility to create plans for community care and support based on what will work best for them.
>
“Compared with previous thinking, a broader recognition emerged that structural approaches – that is, public health programs that promote health where it is produced and reproduced –are not a “nice” accompaniment to ‘the real stuff’ of HIV prevention strategies, but are CENTRAL to them.”
MEASURING PROGRESS
Indicators
Our partners send quarterly updates to our Africa Partnerships team, which give a well-rounded idea of how their communities are doing according to internationally-recognized standards. In the area of HIV stigma and discrimination, it is especially important that HIV response begins in households and in the community. HIV indicators fall into three main buckets:
1. Community Care and Support
Refers to services that holistically address and support HIV/AIDS-related needs and vulnerabilities. These are the non-clinical needs that ultimately impact clinical care and adherence to treatment. We first delved into these in a blog where we introduced HIV indicators, specifically when measuring individuals accessing HIV care, treatment, and support.
2. Health systems strengthening
Activities that aim to strengthen the health sector’s response to HIV and to community needs such as training for employees specifically focused on HIV.
3. Combination Prevention
Programming focused on using a combination of HIV prevention interventions and services across biomedical and behavioral approaches, promoting gender equality and protection of human rights that may perpetuate stigma and discrimination. This aims to reduce the risk of HIV for communities (individuals or small groups) irrespective of their known HIV status. The difference between combination prevention and community care and support is that this focuses on the general population, including people living with HIV, people with unknown statuses, and those who are HIV-negative.
This can include risk assessment, behavioral counseling, and medical referrals for relevant services; HIV testing and counseling (direct or by referral); post-test connection to relevant services; case management and prevention services on disclosure; partner testing; and addressing barriers and facilitating access to biomedical services such as prevention of mother-to-child transmission (PMTCT), antiretroviral therapy (ART), and voluntary male circumcision.
Outputs
1. Individuals reached with interventions explicitly addressing stigma and discrimination.
At the individual level these are services that explicitly address stigma and discrimination to one individual at a time such as counseling and mentorship interventions. For small groups, these are groups of less than 25 people addressing stigma and discrimination through things like empowerment trainings, workshops for target groups on inclusion of people living with HIV, and rights-based education.
At the community level, this directly addresses stigma and discrimination in a community-wide setting with up to 100 people. This doesn’t count mass-marketing messages because these have proven to be ineffective in the current state of HIV/AIDS education. So this level includes things like town hall meetings, raising awareness, and large discussion groups.
2. Institutions reached with intervention that specifically address stigma and discrimination.
This includes institutions like churches, schools, and health facilities that have been newly reached with stigma and discrimination interventions, even if only one individual has been reached that quarter. This includes training, policy development, assessments, campaigns and so on that directly mitigate HIV-related stigma and discrimination.
WHAT DOES THIS LOOK LIKE IN REAL LIFE? | JANE’S MESSAGE
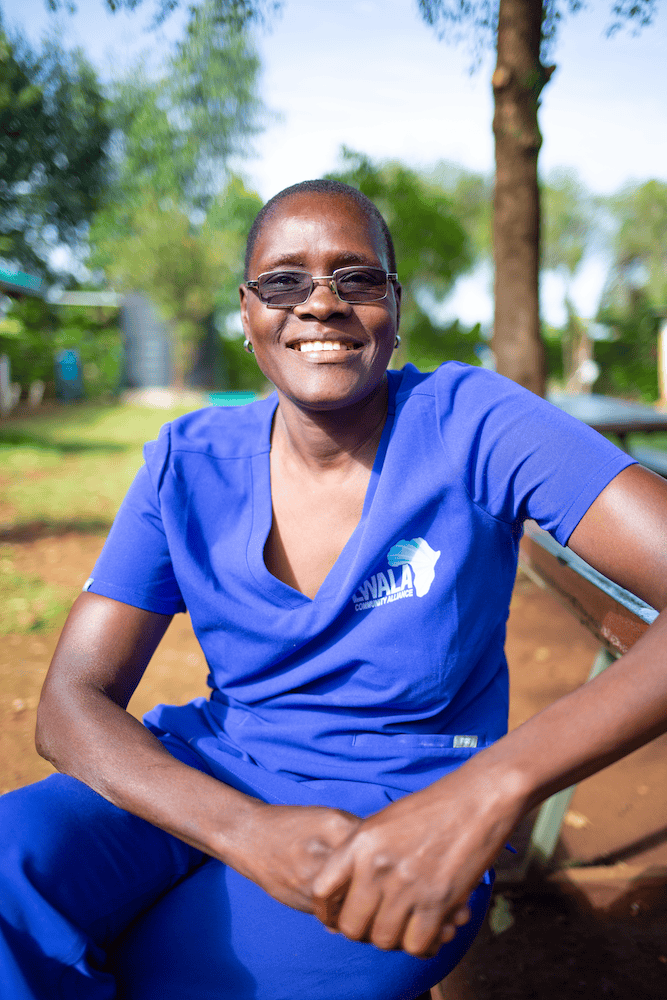
In our previous post on the importance of prevention of mother-to-child transmission of HIV, we introduced Jane. Jane is a mentor mother who has used her own experience of living with HIV to be a role model and leader in her community for other mothers going through the same thing. She says on this subject:
I can say that regarding stigma, he or she should have a positive attitude regarding their status, because this HIV virus is normal like any other illness… It’s just a normal disease, and people should not fear, they should live a normal life and tell their stories also. …
[For someone expressing stigmatizing attitudes,] I can just tell them that HIV doesn’t kill anyone… if your immune system is down, that is when you can be infected with malaria, TB, cyclic diseases, and those diseases are what will kill you. But the virus [itself] doesn’t kill anyone. So someone can just go to their store, take the [HIV] drugs, or if the test is negative, continue to get tested after every 3 months. It is possible for you to stay healthy. As long as you take [HIV] drugs properly and you eat a balanced diet… that is enough.
Jane touches on a very important point that many who perpetuate HIV stigma don’t understand: HIV isn’t what it used to be, and people who have contracted it do not deserve to live a bad life because of their status.
We have worked hard since the beginning of our organization to help spread this message of love and understanding, because we believe the Lord intended for us to do so for all of our brothers and sisters around the world. We praise God for our partners who make it possible for us to do this work in sub-Saharan Africa and for all of you, whose faithful compassion fuels our fight to end the HIV/AIDS and water crises one step at a time.
You may have seen our posts in the past about how our Africa Partnerships (AP) team works with our trailblazing partners in the fields of water, sanitation, and hygiene (WASH) and HIV/AIDS to measure the lifelong change they are creating in their communities. Here is a great post where we introduced what sorts of things they keep track of as part of our participation in the global health community and how those have been perfected over the years to accurately portray strides we make towards worldwide health goals.